By: James Phelps, M.D.
“Bipolar” is the wrong word. Worse than inaccurate — it’s directly misleading:
1. Depression is the main problem for most folks. Bipolar should be called “Depression Plus.”
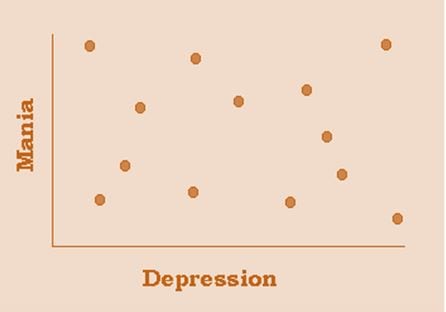
2. Depression and manic symptoms frequently occur together, in “mixed states.”
3. Many people with “unipolar” depression also have manic symptoms.
4. There is no dividing line between “unipolar” and “bipolar.” Prominent mood specialists agree: there are people all along a continuum from plain depression to full Bipolar I.
All of this complexity comes from one thing: subtle hypomania. If you can be a little hypomanic, you can be a little bipolar. You can be a little mixed. You can be a little off your normal and still be “normal” to others’ eyes. Call it “A More Nuanced View of Hypomania”, the topic of a webinar I’ll be presenting for IBPF on September 20th (register here!).
Sound new? Sound radical? Well, you know the DSM, the rule book for diagnoses. No one defends the DSM rules about hypomania as “reality”. The rules are simply agreed-upon cut-offs. But the reality is: hypomania can be short. It can be subtle. It can be almost impossible to detect unless you know – from your own experience – what to look for.
For example, the DSM says it’s not hypomania unless it lasts 4 days. That’s clearly wrong: good data support a cut-off as brief as 2 days. Indeed, there’s been so much experience with even shorter hypomania that it has a name: “ultradian cycling” – more than one mood shift in a single day. So there is no clear minimum duration. The longer a hypomania lasts, the easier it is to tell apart from mood/energy shifts caused by circumstances. But short happens.
Ask someone who really knows their hypomania: it can come on with good news, or a fun gathering with friends. Subtle, but over-energized. Funny, yes, a little too funny though. Later, a little too irritable over minor things. Sure, he was a jerk, but your reaction was a little too strong. If you’d had more sleep last night, you’d have handled it better. Was that really hypomania, or just too little sleep? Oh wait: your friend said you were talking kinda fast too. Not just irritable. Maybe hypomania then?
Does it matter? You bet it does. As you have likely seen: hypomania can lead to a bad depression. Your brief “up” might have been pretty fun there for a while, before the irritable phase, but when the depression comes: definitely not worth it. So, you need more mood stabilizer. Maybe that’s more regular sleep. Maybe that’s less late-night light exposure (you can cheat: you can use the amber lenses – know that story?). Maybe less frequent intense social gatherings, or more downtime in between. All these precede considering turning up your current mood stabilizer medication, or adding another one.
Subtle hypomania also has huge implications for diagnosis. You don’t have to have full hypomania to be bipolar? Unlike pregnancy — you can be “a little bipolar?” Don’t take that from me. Take it from the chairman of the DSM-5. Or the head of the National Institutes of Mental Health (NIMH) Bipolar Spectrum Division. Or the head of the largest bipolar research project ever, the STEP-BD. I’ll show you the references in the webinar September 20th. We’ll spend about 30 minutes considering implications of subtle hypomania; and another 20-30 minutes on your questions. Talk to you then, perhaps…
*To register for Dr. Phelp’s webinar, A More Nuanced View of Hypomania, and an oppurtunity to ask him questions afterwards, please click here!*
James Phelps, M.D. has specialized in bipolar spectrum variations for over 15 years. He has authored multiple peer-reviewed articles on mood disorders, and serves as Bipolar section editor for Psychiatric Times. His no-profit website, PsychEducation.org, focuses on complex bipolar variations; it has received over a million visitors. He accepts no honoraria from pharmaceutical companies, but does receive royalties from McGraw-Hill and W.W. Norton for books on the bipolar spectrum. A Spectrum Approach to Mood Disorders, 2016 from Norton, is for professionals; Bipolar, Not So Much , also 2016 from Norton, is for patients and families.