Author: Brooke Rowland
Maslow’s Hierarchy of Needs provides helpful structural guidance for the multi-faceted approach to treating Bipolar Disorder. Articulated in 1943, his theory stated that our needs can be visualized as a pyramid and that the needs at the bottom of the hierarchy are fundamental to our survival. As those base needs are met, we can achieve the next needs in the pyramid which become more social and psychological in nature. Similarly, in the treatment of Bipolar Disorder, more “base” and fundamental needs must be tended to before proceeding to more dynamic and in-depth psychotherapies. This blog post will outline this tiered approach while providing brief overviews and links to further information.
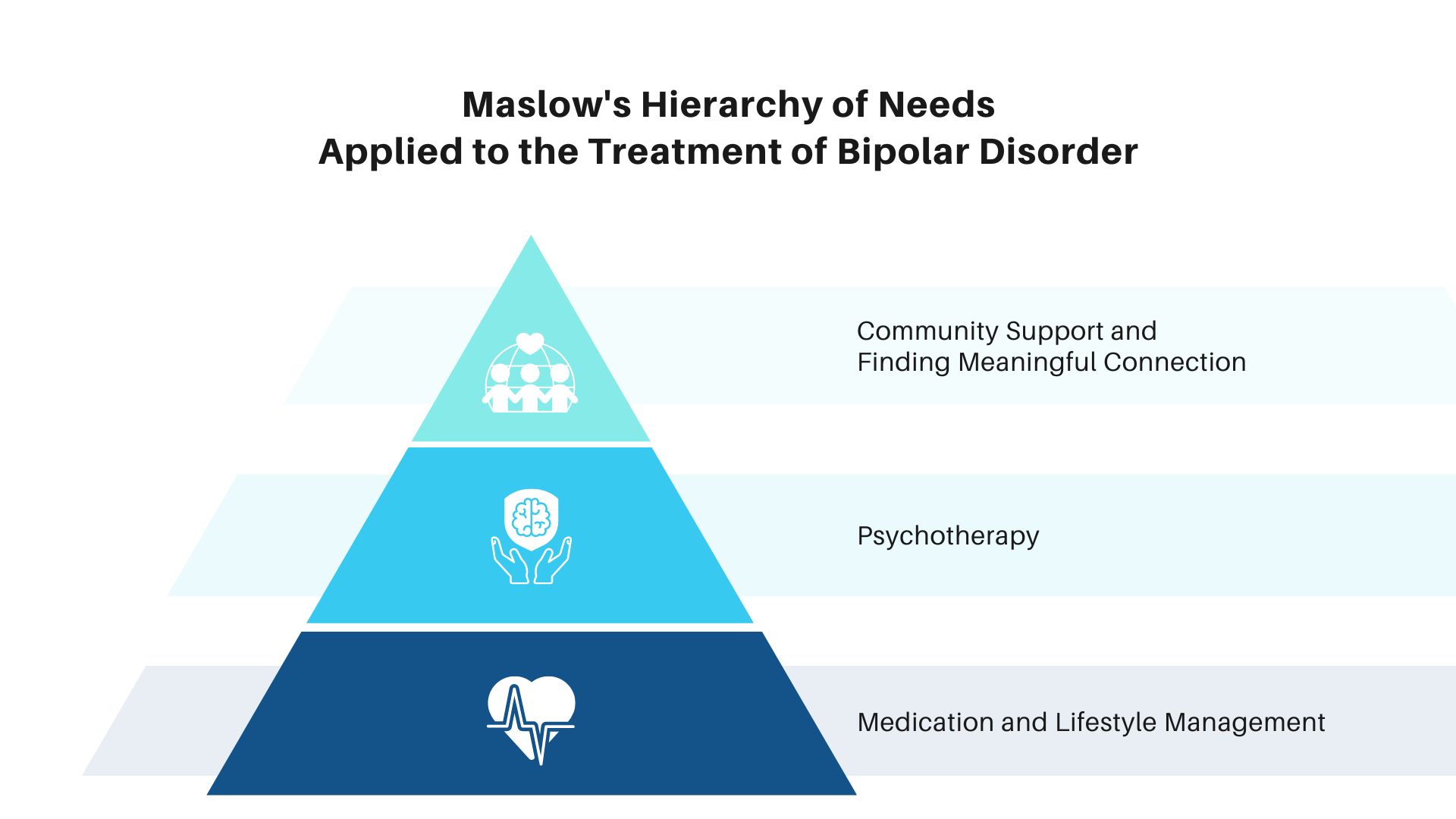
Tier 1: Medication and Lifestyle Management
Medication
Research establishes that Bipolar Disorder is a lifelong condition that requires medication management even during periods of stability (Treatment of Bipolar Disorder). It is highly recommended that individuals living with Bipolar Disorder meet with a psychiatric medical professional to be assessed for medication management. There are various options for medications including mood stabilizers, anti-psychotics, anti-depressants when used in combination with a mood stabilizer, and other medications that target sleep and anxiety.
Lifestyle Management
In terms of building a healthy foundation for stability and wellness, it is important to consider the following lifestyle factors: sleep, nutrition, movement/physical activity, abstaining from alcohol or recreational substances, and lifestyle tracking.
● Sleep: Sleep disturbances are linked to mood dysregulation, poorer outcomes, and relapse in Bipolar Disorder (The Role of Sleep in Bipolar Disorder). It’s therefore important to have an understanding of sleep hygiene. Some basic principles of sleep hygiene include
○ Establishing a consistent sleep/wake schedule
○ Making sure your bedroom is conducive to sleep (e.g., quiet, dark, comfortable temperature, limited electronic devices)
○ Establishing a relaxing “wind down” bedtime routine
○ Avoiding large meals, caffeine, and alcohol before bedtime
○ Using your bed only for sleep and sex
○ Going to bed when tired (If you don’t fall asleep within 20 minutes, get out of bed and do something to help you unwind until you’re tired enough to return to bed)
○ Limiting napping or avoiding it altogether
● Nutrition: While there is no specific recommended diet for Bipolar Disorder, it is nonetheless important to eat a balanced diet of protective, nutrient-dense foods. Some research establishes that getting omega-3 fatty acids found in fish oil may be helpful (Omega-3 for bipolar disorder: meta-analyses of use in mania and bipolar depression). It is important to avoid excess amounts of caffeine and make sure to follow your doctor’s instructions to stay away from foods that may impact your specific bipolar medication.
● Movement: The Anxiety and Depression Association of America recommends that individuals living with Bipolar Disorder engage in physical activity for 30 minutes, 3 to 5 days per week (ADAA Tips). Make sure to talk to your doctor before starting a new routine, stop any activity that makes symptoms worse, and pay attention to any manic symptoms that may increase after starting a new exercise routine.
● Alcohol/Substance Use: It is recommended to avoid recreational drugs and alcohol. If you do use recreational substances while taking medication, make sure to discuss this openly with your treatment providers so you can understand its impact on mood and any medication interactions. Marijuana use is associated with worsened affective episodes, psychotic symptoms, rapid cycling, suicide attempts, decreased long-term remission, poorer global functioning, and increased disability (Effects of Marijuana on Mental Health: Bipolar Disorder). Alcohol use can worsen the risk of mood swings, depression, violence, and suicide (Bipolar disorder and alcoholism: Are they related?).
● Tracking: Tracking your daily mood symptoms, sleep, medication compliance, and life events can provide insightful data to understand triggers and helpful treatment. Some helpful tracking apps include: eMoods Bipolar Mood Tracker, Daylio, and Moodfit.
Tier 2: Psychotherapy
There are various forms of psychotherapy (“talk therapy”) that can be helpful for managing Bipolar Disorder. Here are some options:
● Cognitive Behavioral Therapy: CBT is a form of therapy that examines and targets unhelpful ways of thinking and patterns of behavior in order to relieve symptoms and become more effective in life. It is based on the idea that your thoughts, feelings, physical sensations, and actions are all interconnected and that distorted or negative thinking patterns and feelings can trap you in a negative cycle (Thought Record CBT Exercise).
● Dialectical Behavioral Therapy: DBT is rooted in the core belief that opposite things can be true at the same time. The core dialectic in this treatment is between “acceptance and change.” DBT is comprised of 4 modules: Mindfulness, Distress Tolerance, Interpersonal Effectiveness, and Emotion Regulation.
● Psychoeducation: Learning about Bipolar Disorder can help you and your loved ones gain greater understanding and can help identify issues, make a relapse-prevention plan, and help you get the best support to stick with treatment.
● Eye Movement Desensitization Reprocessing (EMDR): EMDR is a form of treatment using bilateral stimulation that helps individuals process and heal from trauma and other distressing life experiences. If someone with Bipolar Disorder is struggling with unresolved trauma, they may benefit from EMDR so as to reduce the potential that trauma triggers may lead to mood episodes. (Eye Movement Desensitization and Reprocessing (EMDR) Therapy).
● Interpersonal and Social Rhythm Therapy (IPSRT): IPSRT focuses on the regulation and stabilization of daily rhythms (e.g., sleeping, waking, exercise, and mealtimes). It is based on the idea that a consistent routine allows for better mood management.
● Family-Focused Therapy: Involving family in treatment can increase support and improve communication in order to help you stick with your treatment plan and also recognize and manage early warning signs of mood swings.
● Mindfulness: Two particularly helpful forms of mindfulness practice include Mindfulness-Based Stress Reduction (MBSR) and Mindful Self-Compassion (MSC). MBSR is an eight-week evidence-based program that offers secular and intensive mindfulness training to assist with stress, anxiety, depression, and pain (MBSR 8-Week Online Live). MSC is a combination of mindfulness and compassion training designed to enhance the capacity for self-compassion (Mindful Self-Compassion (MSC)).
Tier 3: Community Support and Finding Meaningful Connection
Being diagnosed with Bipolar Disorder can sometimes feel scary, alienating, and isolating. We recommend connecting with local advocacy organizations to meet like-minded individuals. Fostering a sense of community can provide a sense of empowerment for individuals living with bipolar disorder and their caregivers. This is where the IBPF can help! You can connect with IBPF on social media (Facebook, Instagram, LinkedIn, Youtube) to join a community of people dedicated towards seeking support and giving support to those in need.
Overview of Levels of Care
When someone begins their journey to treatment for Bipolar Disorder, there are various options in terms of where they can receive the treatment recommendations outlined above. Care can be provided at the outpatient level of care (in both individual and group settings), Intensive Outpatient Programs (IOP), Partial Hospitalization Programs (PHP), residential treatment centers, and inpatient psychiatric hospitals. We recommend consulting with your treatment providers to see which level of care makes the most sense for you.
Brooke Rowland is a passionate advocate for individuals suffering from addiction and mental illness. She holds a Masters Degree in Social Work from USC, a Juris Doctorate from Loyola Law School, and a Bachelors of Arts from UC Berkeley in History. Brooke also spent an intensive year studying abroad at Magdalen College, Oxford University and is a member of the California Bar Association. Learn more about Brooke here!
The content of the International Bipolar Foundation blogs is for informational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician and never disregard professional medical advice because of something you have read in any IBPF content.


