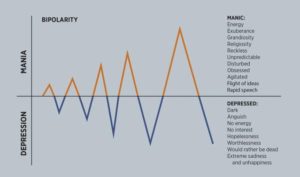
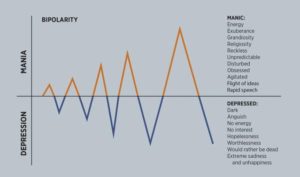
Formerly known as “manic depressive illness,” bipolar disorder is a term that, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), comprises a cluster of related disorders that are characterized by distinctive and extreme shifts, or cycles, in mood. These moods oscillate between varying degrees of two poles: mania and depression.
Mania is marked by elevated, expansive, or irritable moods and increased energy; feeling overly happy and optimistic; being highly talkative but with pressured speech; or having inflated self-esteem and/or feeling grandiose or religious, as if on a mission directly from God.
There’s often little need for sleep, but the mind is always racing with ideas and distracted, which can lead to high-risk, dangerous, or painful activities.
Mania can be life-threatening and destructive, causing marked social or occupational impairment or hospitalization to prevent harm to self or others. It is driven largely by the over-production of chemicals that create and regulate mood.
Depression often results in decreased energy, diminished interest, worthlessness, hopelessness, lack of focus, and recurrent thoughts of death. The person feels sad and empty and often has a significant change in weight or appetite.
 Source: Gregg Martin, Kristi Choate, and Julie Coffey with assistance from “Proceedings” staff
Source: Gregg Martin, Kristi Choate, and Julie Coffey with assistance from “Proceedings” staff
Medical depression is a life-threatening condition that inspires recurrent thoughts of suicide. As the opposite of mania, it is largely driven by the under-production of those same critical chemicals that create and regulate mood.
Bipolar disorder and other mental illnesses are real physical illnesses that occur within the brain. They are not the “fault” of the afflicted person or evidence of moral failings, flawed character, or a cut and dry lack of willpower. So we must treat them as we would a person with cancer or diabetes—recognize it, get medical help, diagnose it, treat it, heal it, and get them back to a healthy life.
Hyperthymia helped fuel my success
My first four decades of life were healthy, happy, and successful, from childhood through West Point and throughout most of my military career. I was an accomplished student, athlete, and leader, known for high levels of energy, enthusiasm, and drive.
I completed the Army’s elite and grueling Ranger school, ran seven marathons (each under three hours, including a 2:36), and completed a Ph.D. at the Massachusetts Institute of Technology, plus much more; all while happily married and helping my wonderful wife raise our three talented sons.
I recently learned that I benefited from what psychiatrists call “hyperthymia,” or a “hyperthymic temperament.” This means that I was in a near-continual state of mild mania, which gave me abnormally high levels of energy, drive, enthusiasm, extroversion, happiness, optimism, positivity, and the like.
This psychiatric condition, which is below the level of a mental illness, lasted from my teenage years into my forties. It elevated into bipolar disorder, then full-blown mania, crippling depression, and terrifying psychosis from 2003 to 2016, and has since returned. (Note that hyperthymia is typically distinct from “hypomania,” which is episodic—vs. continual—states of mild mania.)
Hyperthymia helped fuel my success by amplifying my natural abilities and talents. This condition is well explained in acclaimed psychiatrist Dr. Nassir Ghaemi’s fascinating book, A First-Rate Madness: Uncovering the Links Between Leadership and Mental Illness.
My hyperthymic personality put me in good company, with former presidents John F. Kennedy and Franklin D. Roosevelt. But on the downside, it put me at greater risk of developing bipolar disorder, full-blown mania, and anxiety disorder, which is precisely what happened.
Activation of bipolar disorder
In 2003, something seriously changed. I thrived while commanding a combat engineer brigade of more than 10,000 soldiers in the Iraq War, including the attack on Baghdad and beyond.
The more intense the pressure, stress, and danger, the happier, more exuberant, energetic, and enthusiastic I became. Indeed, I had never felt so alive, focused, and high on life as while leading soldiers in combat. I marveled at the courageous and amazing things our engineers did on the battlefield. Perhaps this confession alone is evidence of mental illness.
But either way, my combat euphoria—like other chemical intoxicants—would have long-lasting physical effects on my brain, particularly the neurological circuitry and elements responsible for producing and regulating the mood-related chemicals of dopamine and endorphins. Too much of these chemicals creates mania and too little leads to depression.
What I did not realize at the time was that this fabulous euphoria and “high” were my brain’s response to the intense elevation of stress, a high-performing state of mania. My doctors have determined that my genetic predisposition for bipolar disorder was activated by the intense stress of war. I suddenly went from having a latent bipolar potential to actual, activated bipolar disorder.
This Iraq War “triggering event” is the confirmed opinion of the Army Medical Department and the Department of Veterans Affairs in their medical analysis and assessments of my condition.
But at the time, no one, myself included, knew any of that. In fact, extra energy, enthusiasm, focus, and creativity generated by my high-performing mania significantly enhanced my performance in combat. I felt like I was a kind of Superman—fearless, overflowing with confidence, able to accomplish or do anything. But feeling like Superman should have been a warning sign.
Over the next decade, my performance and recognition by my superiors continued to rise. I was promoted twice and assigned to increasingly complex and difficult assignments in the Army.
Yet during this time—most of which I was a general officer—my manic highs surged higher and depressive lows sank lower. Meanwhile, neither my family, friends, work colleagues, nor my doctors had any idea that I was afflicted with a brain malady, let alone bipolar disorder.
Anonymous complaints eventually made their way to my boss. And by the time my family realized something was seriously wrong, I had been forced to resign from the presidency of the National Defense University (NDU).
Soon, the moon of depression would eclipse the sun of mania.
A version appeared in “Task & Purpose” and “Psychology Today
If you or someone you love is contemplating suicide, seek help immediately. For help 24/7 dial 988 for the National Suicide Prevention Lifeline, or reach out to the Crisis Text Line by texting TALK to 741741. To find a therapist near you, visit the Psychology Today Therapy Directory.
The content of the International Bipolar Foundation blogs is for informational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician and never disregard professional medical advice because of something you have read in any IBPF content.
 Source: Gregg Martin, Kristi Choate, and Julie Coffey with assistance from “Proceedings” staff
Source: Gregg Martin, Kristi Choate, and Julie Coffey with assistance from “Proceedings” staff

