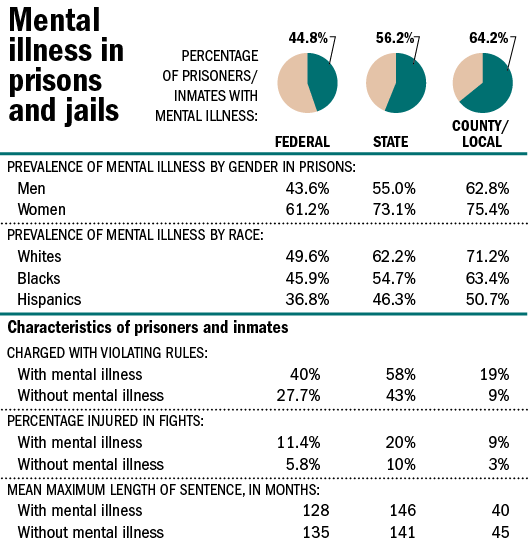
Mentally ill persons increasingly receive care provided by correctional agencies. In 1959, nearly 559,000 mentally ill patients were housed in state mental hospitals (Lamb, 1998). A shift to “deinstitutionalize” mentally ill persons had, by the late 1990s, dropped the number of persons housed in public psychiatric hospitals to approximately 70,000 (CorrectCare, 1999). As a result, mentally ill persons are more likely to live in local communities. Some come into contact with the criminal justice system. In a 2006 Special Report, the Bureau of Justice Statistics (BJS) estimated that 705,600 mentally ill adults were incarcerated in state prisons, 78,800 in federal prisons and 479,900 in local jails. In addition, research suggests that “people with mental illnesses are overrepresented in probation and parole populations at estimated rates ranging from two to four times the general population” (Prins and Draper, 2009). Growing numbers of mentally ill offenders have strained correctional systems. (See more here)
I have used portions of this quote on other blogs here because it is a shocking paragraph drawn from the annals of the National Institute of Corrections. What can we do about people with mental illness in the justice system? Why does the justice system treat them so differently? What is being done to change that?
Today I got out of a six-day jail stay, preceded by a one-week hospital stay. Having checked myself into a facility for suicidal depression two weeks ago, I missed court and was believed to have absconded. Well, why didnt I just tell someone I was going? For the same reasons I failed to take my meds for a month, soothed by relief from depression in moments of mixed hypomania. The same thoughts (or lack thereof) that were at work when I picked up drugs to ease the (easily foreseeable by outsiders) resulting deep depression from lack of medication. Those made me dig a deeper and deeper hole for myself.
This all is very specific to me, my bipolar disorder and my pathways, however, it emerges from a seasonal change that happens every year. In early October a friend texted me:
How are you doing?
Fine. Why?
This is the time of year you tend to (mess) things up for yourself, my ex of 7 years proclaimed.
Then I looked back (I was well into mental health relapse and on the way to addiction relapse by this time) over my 46 years. It was epiphanic: For at least 20 years I could see it, the repeated, almost annual, hospitalizations, break downs, job losses, relationships ending, suicidal, self-destructive patterns.
It all started with stopping my medicine. Then stopping or missing treatment. Then, inevitably, drug use to mask the symptoms (producing a myriad of negative consequences). I commented to my therapist that I just wanted to feel something again. When they got my meds right I did feel something: fear and sadness about the consequences of my behaviors. Cold handcuffs and a jail that I need not have been in until I was more stable.
“Are our prisons’ rehabilitative services set up to provide comprehensive mental health and psychiatric programs to deal with the increasing population with such severe psychopathology and impairment? Shouldn’t standards of care of psychiatric disorders be respected in the correctional setting as they are in other community provider settings? Shouldn’t inmates have access to the same standard of treatment consistent with the principle of equivalence?
Shouldn’t access to specialized diagnostic procedures and assessment protocols, including general and neuropsychological testing, be available and applied to identify neuropsychiatric and behavioral consequences of brain injury and other organic disorders? Are states willing to allocate sufficient budget and manpower resources to meet the needs of mentally ill and substance abusing offenders? Are legislators and administrators willing to take a serious look at the criminal justice process to determine how to refer mentally ill arrestees and offenders to various treatment programs?”
Dr. Daniels article, from which the query above comes, alludes to privatization of mental health care in jails and prisons. I have experienced the difference in privatized vs non-privatized care and found the former is superior. The big caveat? As I sat in a very small room with 20 other females in our county jail awaiting first appearance, one of the ladies experienced a panic attack. When she left the room suddenly and wouldnt return, she was physically put on the ground by first the Corrections Officer and very quickly, the Detention Response Team (which are the bad boys of jails the ultimate take down SWAT team of incarceration). She was brought to the judge in cuffs and subdued. You cant privatize the Correction Officers (COs) and Response Teams. They are corrections minded and they are the first responders to altercations daily.
Another of my fellow inmates was a young lady with Severe PTSD and bipolar disorder who Drug Court personnel took extra time in explaining to her the sentence she had just received (she was sentenced to a Mental Health Assessment and treatment rather than addiction treatment at this juncture). While the Drug Court Public Defender talked in soothing tones to her, moments later a sheriff said I hate to break this up ladies but we need to be somewhere. COs need to be trained for dealing with inmates who have severe mental illness.
I spoke, at length, with this woman and assured her that her sentence was in her best interest. She confided that she was feeling very messed up and confused and she would try and see it as a good thing, as we were suggesting it was. Have hope, my fruenda. I told her. I could offer nothing more, but I said a prayer that she wouldnt have a panic attack and be man handled.
What really drives the difference in that and the mental hospital I was at the week prior were the little things. An extra moment of reexamination, a well-timed hug, a softer approach. That, not the food or decorations at the hospital, set it apart from the jail.
Right after college I worked in a halfway house for nonviolent offenders and was told I was hired for my counseling side. I hire half of you counseling minded and half correction minded. I was told this and wondered why we all couldnt be both. Corrections would argue that, in those first minutes of crisis, it is imperative to take control from individuals who are losing or out of control. Counseling teaches us to be calm and non-threatening in these critical moments. Two people have died nearby after being severely mistreated by correctional staff, yet we still debate it in the halls of academia as though at war between corrections-minded and counseling-minded individuals and bodies of people is okay.
Advocates for Better MH Treatment in Corrections Resources:
- Treatment and Advocacy Center
- Prison Policy Initiative
- Advocates for People With Mental Illness
- Unite to Face Addiction
As well as many state organizations and initiatives.
As I have stated in the past, be an advocate for people incarcerated with a mental illness. Let your voices be heard so that we can bring reform!
Read the rest of Liz’s posts here.


